Ovulatory cycle (human)
The normal ovulatory cycle in women is a complex and important process which repeats throughout the childbearing years. The cycle centers on the release of a mature oocyte from the ovary, and it is this event that is a basic determinant of female fertility. During the cycle, the lining of the uterus,[[called the endometrium, changes to accomodate the possibility of implantation of a zygote. "Zygote" is a scientific name for the fertilized ovum, and is the single cell that is the very earliest stage of an embryo. If no pregnancy is established, this lendometrial lining is shed as menstrual blood; and the cycle repeats. Since the most dramatic outward evidence of these events is menstruation, the events of the cycle are often referred to as the "menstrual cycle'. Technically, it is possible to have an "anovulatory" menstrual cycle in which no egg is produced (see menarche), but both terms are used correctly to describe the periodic ovulation and shedding of endometrial lining by women through the childbearing years.
There are several hormones that play vital roles in the ovulatory cycle, some produced by the ovaries themselves, others from the pituitary gland and from the part of the brain known as the hypothalmus.These hormones are described in the table below.
- estradiol (estrogen)
- follicle-stimulating hormone (FSH)- - anterior pituitary gland-a gonadotropin
- inhibin-glycoprotein-granulosa and luteal cells of the ovary-suppresses follicle-stimulating hormone (FSH) secretion
- leutinizing hormone (LH)- - anterior pituitary gland -a gonadotropin
- progesterone
Hormonal events of the normal ovulatory cycle
The hypothalamus secretes pulses of gonadotropin-releasing hormone (GnRH) continuously, throughout the cycle.
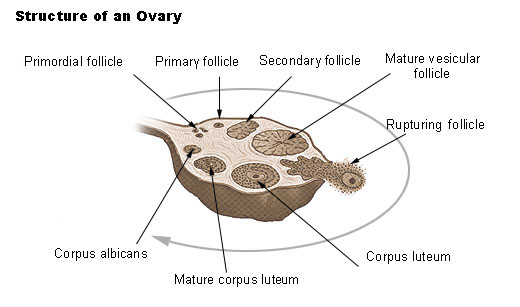
(1) Rising follicle-stimulating hormone (FSH) levels cause follicular recruitment.T(2) Follicular development causes an increase in estradiol levels.
(3) Increasing estradiol levels, secreted by maturing follicles, cause endometrium proliferation and important changes in the cervix:the amount of mucus secreted by the cervical epithelium increases, its consistancy changes, and opening of the cervical os increases.
(4) Follicular dominance occurs in the ovary
(5) Estrogen together with inhibin shuts off FSH, so that no new follicles are recruited. The dominant follicle of the ovary that will ovulate this cycle continues growing.
(6) Estrogen is secreted by the dominant follicle, the rising blood levels of estrogen feeds back negatively on the hypothalamo- pituitary axis.
(7) Pituitary LH rises a peak initiates luteinization of the follicle. The ovum is released from the follicle, and enters the fallopian tube on its way to the uterus. The ovum has 12 to 24 hours of life as a gamete, and during that time will either be fertilzed or will die.
(8) Secretion of progesterone begins in the follicle with leutinization. This first rise in progesterone level maintains the plateau of LH during the LH peak.
(9) The high plateau of LH secretion helps maintain a normal corpus luteum, and an adequate luteal phase of the menstrual cycle.
(10) The corpus luteum produces both progesterone and estrogen.
(11) Progesterone changes the lining of the uterus (endometrium) and the cervical mucus. The endometrium becomes the secretory type. The cervical mucus, changes from estrogenic to progestational type. If fertilization has not occurred, the corpus luteum begins to regress after 6–7 days, tapers off secretion of estrogen and progesterone.
(12) Estrogen and progesterone levels return to early follicular phase levels approximately 14 days after the corpus luteum first had formed.
(13) This drop in sex hormone levels releases the suppression of FSH and LH on the hypothalamo- pituitary axis. Go to (1), a new cycle has begun.