Diabetic foot: Difference between revisions
imported>Robert Badgett |
imported>Robert Badgett |
||
| Line 38: | Line 38: | ||
| Litzelman<ref name="pmid8498761"/><br/>1993|| 395 patients<br/>• general medicine practice|| Patient and provider education||Usual care||• Any foot lesion<br/> • Serious foot lesions at one year|| Not reported||• 11%<br/>• 2.9%||<br/>• Insignificant <br/>• Significant reduction | | Litzelman<ref name="pmid8498761"/><br/>1993|| 395 patients<br/>• general medicine practice|| Patient and provider education||Usual care||• Any foot lesion<br/> • Serious foot lesions at one year|| Not reported||• 11%<br/>• 2.9%||<br/>• Insignificant <br/>• Significant reduction | ||
|- | |- | ||
| McCabe<ref name="pmid9472868"/><br/>1998|| 2002 patients<br/>• high-risk<br/>• general diabetic | | McCabe<ref name="pmid9472868"/><br/>1998|| 2002 patients<br/>• high-risk<br/>• general diabetic clinic|| Screening and referral to foot-care clinic if they had prior ulcer, had low ankle–brachial index (<0.75), or had foot deformities||Usual care||• Ulceration within 2 years<br/>• Amputation rates|| • 2%<br/>• 0.1%|| 4%<br/>1.2%||• Insignificant<br/>• Significant | ||
|- | |- | ||
| Lincoln<ref name="pmid18758747"/><br/>2008|| 172 patients<br/>• prior ulceration<br/>• specialist clinic|| Targeted, one-to-one education ||Usual care||Re-ulceration at<br/>• 1 year<br/>2 years|| • 30%<br/>• 41%||• 20%<br/>• 41%||• Insignificant<br/>• Insignificant | | Lincoln<ref name="pmid18758747"/><br/>2008|| 172 patients<br/>• prior ulceration<br/>• specialist clinic|| Targeted, one-to-one education ||Usual care||Re-ulceration at<br/>• 1 year<br/>2 years|| • 30%<br/>• 41%||• 20%<br/>• 41%||• Insignificant<br/>• Insignificant | ||
Revision as of 20:45, 9 September 2012
The diabetic foot is "common foot problems in persons with diabetes mellitus, caused by any combination of factors such as diabetic neuropathies; peripheral vascular diseases; and infection. With the loss of sensation and poor circulation, injuries and infections often lead to severe foot ulcers, gangrene and amputation."[1]
Diagnosis
The signs of underlying osteomyelitis are "an ulcer area larger than 2 cm2, a positive probe-to-bone test result, an erythrocyte sedimentation rate of more than 70 mm/h, and an abnormal plain radiograph" according to a systematic review by the Rational Clinical Examination.[2] A normal magnetic resonance imaging makes osteomyelitis unlikely.
The National Institute for Health and Clinical Excellence (NICE) has addressed screening and recommends annually:[3][4]
Physical examination of patients’ feet:
- testing of foot sensation using a 10 g monofilament or vibration
- palpation of foot pulses
- inspection of any foot deformity and footwear
Although NICE and others[5][6] have recommended monofilament testing, its contribution in the major randomized controlled trials is not clear.[7][8]
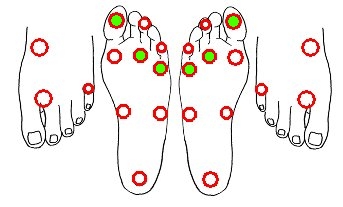
If screening with the monofilament is done, a three site test of the plantar surfaces of the great toe, the third metatarsal, and the fifth metatarsalsis is adequate according to a systematic review[9] of studies[10]. Another systematic review questions the test accuracy of the monofilament exam.[11]
The role of patient education in preventing foot ulcers is not clear according to the Cochrane Collaboration. [12]
Prevention
"Integrated foot risk scores are more sensitive than individual clinical criteria in predicting future foot ulceration and are likely to be better screening tools." [13]
An example of a foot risk score is the Scottish foot ulcer risk score. Low risk is defined as able to detect at least one pulse per foot, and able to feel 10 g monofilament, and no foot deformity, physical, or visual impairment. The negative predictive value of a 'low-risk score' is 99%. [14]
| Trial | Patients | Intervention | Comparison | Outcome | Results | Comment | |
|---|---|---|---|---|---|---|---|
| Intervention | Control | ||||||
| Reiber[8] 2002 |
400 patients • foot ulcer • Excluded severe deformity |
Therapeutic shoes | Usual footwear | Re-ulceration | 15% | 17% | Insignificant difference |
| Litzelman[7] 1993 |
395 patients • general medicine practice |
Patient and provider education | Usual care | • Any foot lesion • Serious foot lesions at one year |
Not reported | • 11% • 2.9% |
• Insignificant • Significant reduction |
| McCabe[15] 1998 |
2002 patients • high-risk • general diabetic clinic |
Screening and referral to foot-care clinic if they had prior ulcer, had low ankle–brachial index (<0.75), or had foot deformities | Usual care | • Ulceration within 2 years • Amputation rates |
• 2% • 0.1% |
4% 1.2% |
• Insignificant • Significant |
| Lincoln[16] 2008 |
172 patients • prior ulceration • specialist clinic |
Targeted, one-to-one education | Usual care | Re-ulceration at • 1 year 2 years |
• 30% • 41% |
• 20% • 41% |
• Insignificant • Insignificant |
Other trials of lesser quality are available.[17] [18]
"Of all methods proposed to prevent diabetic foot ulcers, only foot temperature-guided avoidance therapy was found beneficial in RCTs" according to a meta-analysis.[19] Three trials are available.[20]
Treatment
"Currently there is no research evidence to suggest that any type of hydrocolloid wound dressing is more effective in healing diabetic foot ulcers than other types of dressing" according to the Cochrane Collaboration. [21]
"There is some evidence to suggest that hydrogel dressings are more effective in healing (lower grade) diabetic foot ulcers than basic wound contact dressings however this finding is uncertain due to risk of bias in the original studies" according to a meta-analysis by the Cochrane Collaboration. [22]
References
- ↑ Anonymous (2025), Diabetic foot (English). Medical Subject Headings. U.S. National Library of Medicine.
- ↑ Sonia Butalia et al., “Does This Patient With Diabetes Have Osteomyelitis of the Lower Extremity?,” JAMA 299, no. 7 (February 20, 2008): 806-813.
- ↑ (2004) CG10 Type 2 diabetes - footcare. National Institute for Health and Clinical Excellence
- ↑ Kaiser Permanente Care Management Institute. Guidelines for the management of adult diabetes in Primary Care. Oakland (CA): Kaiser Permanente Care Management Institute; 2006. 10 p. National Guidelines Clearinghouse
- ↑ Singh N, Armstrong DG, Lipsky BA (2005). "Preventing foot ulcers in patients with diabetes.". JAMA 293 (2): 217-28. DOI:10.1001/jama.293.2.217. PMID 15644549. Research Blogging.
- ↑ Kanji JN, Anglin RE, Hunt DL, Panju A (2010). "Does this patient with diabetes have large-fiber peripheral neuropathy?". JAMA 303 (15): 1526-32. DOI:10.1001/jama.2010.428. PMID 20407062. Research Blogging. Review in: Ann Intern Med. 2010 Oct 19;153(8):JC4-10
- ↑ 7.0 7.1 7.2 Litzelman DK, Slemenda CW, Langefeld CD, Hays LM, Welch MA, Bild DE et al. (1993). "Reduction of lower extremity clinical abnormalities in patients with non-insulin-dependent diabetes mellitus. A randomized, controlled trial.". Ann Intern Med 119 (1): 36-41. PMID 8498761.
Cite error: Invalid
<ref>tag; name "pmid8498761" defined multiple times with different content - ↑ 8.0 8.1 8.2 Reiber GE, Smith DG, Wallace C, Sullivan K, Hayes S, Vath C et al. (2002). "Effect of therapeutic footwear on foot reulceration in patients with diabetes: a randomized controlled trial.". JAMA 287 (19): 2552-8. PMID 12020336. [e]
- ↑ 9.0 9.1 Feng Y, Schlösser FJ, Sumpio BE (2009). "The Semmes Weinstein monofilament examination as a screening tool for diabetic peripheral neuropathy.". J Vasc Surg 50 (3): 675-82, 682.e1. DOI:10.1016/j.jvs.2009.05.017. PMID 19595541. Research Blogging.
- ↑ Smieja M, Hunt DL, Edelman D, Etchells E, Cornuz J, Simel DL (1999). "Clinical examination for the detection of protective sensation in the feet of diabetic patients. International Cooperative Group for Clinical Examination Research.". J Gen Intern Med 14 (7): 418-24. PMID 10417599. PMC PMC1496604.
- ↑ Dros J, Wewerinke A, Bindels PJ, van Weert HC (2009 Nov-Dec). "Accuracy of monofilament testing to diagnose peripheral neuropathy: a systematic review.". Ann Fam Med 7 (6): 555-8. DOI:10.1370/afm.1016. PMID 19901316. PMC PMC2775618. Research Blogging.
- ↑ Dorresteijn JA, Kriegsman DM, Assendelft WJ, Valk GD (2010). "Patient education for preventing diabetic foot ulceration.". Cochrane Database Syst Rev (5): CD001488. DOI:10.1002/14651858.CD001488.pub3. PMID 20464718. Research Blogging.
- ↑ Leese GP, Cochrane L, Mackie AD, Stang D, Brown K, Green V (2011). "Measuring the accuracy of different ways to identify the 'at-risk' foot in routine clinical practice.". Diabet Med 28 (6): 747-54. DOI:10.1111/j.1464-5491.2011.03297.x. PMID 21418097. Research Blogging.
- ↑ Leese GP, Reid F, Green V, McAlpine R, Cunningham S, Emslie-Smith AM et al. (2006). "Stratification of foot ulcer risk in patients with diabetes: a population-based study.". Int J Clin Pract 60 (5): 541-5. DOI:10.1111/j.1368-5031.2006.00899.x. PMID 16700850. Research Blogging.
- ↑ 15.0 15.1 McCabe CJ, Stevenson RC, Dolan AM (1998). "Evaluation of a diabetic foot screening and protection programme.". Diabet Med 15 (1): 80-4. DOI:<80::AID-DIA517>3.0.CO;2-K 10.1002/(SICI)1096-9136(199801)15:1<80::AID-DIA517>3.0.CO;2-K. PMID 9472868. <80::AID-DIA517>3.0.CO;2-K Research Blogging.
- ↑ 16.0 16.1 Lincoln NB, Radford KA, Game FL, Jeffcoate WJ (2008). "Education for secondary prevention of foot ulcers in people with diabetes: a randomised controlled trial.". Diabetologia 51 (11): 1954-61. DOI:10.1007/s00125-008-1110-0. PMID 18758747. Research Blogging.
- ↑ Uccioli L, Faglia E, Monticone G, Favales F, Durola L, Aldeghi A et al. (1995). "Manufactured shoes in the prevention of diabetic foot ulcers.". Diabetes Care 18 (10): 1376-8. PMID 8721941. [e]
- ↑ Malone JM, Snyder M, Anderson G, Bernhard VM, Holloway GA, Bunt TJ (1989). "Prevention of amputation by diabetic education.". Am J Surg 158 (6): 520-3; discussion 523-4. PMID 2589581. [e]
- ↑ Arad Y, Fonseca V, Peters A, Vinik A (2011). "Beyond the Monofilament for the Insensate Diabetic Foot: A systematic review of randomized trials to prevent the occurrence of plantar foot ulcers in patients with diabetes.". Diabetes Care 34 (4): 1041-6. DOI:10.2337/dc10-1666. PMID 21447666. PMC PMC3064020. Research Blogging.
- ↑ Armstrong DG, Holtz-Neiderer K, Wendel C, Mohler MJ, Kimbriel HR, Lavery LA (2007). "Skin temperature monitoring reduces the risk for diabetic foot ulceration in high-risk patients.". Am J Med 120 (12): 1042-6. DOI:10.1016/j.amjmed.2007.06.028. PMID 18060924. Research Blogging.
- ↑ Dumville JC, Deshpande S, O'Meara S, Speak K (2012). "Hydrocolloid dressings for healing diabetic foot ulcers.". Cochrane Database Syst Rev 2: CD009099. DOI:10.1002/14651858.CD009099.pub2. PMID 22336859. Research Blogging.
- ↑ Dumville JC, O'Meara S, Deshpande S, Speak K (2011). "Hydrogel dressings for healing diabetic foot ulcers.". Cochrane Database Syst Rev 9: CD009101. DOI:10.1002/14651858.CD009101.pub2. PMID 21901730. Research Blogging.