Abdominal aortic aneurysm: Difference between revisions
imported>Robert Badgett (Undo revision 100512851 by Robert Badgett (Talk)) |
mNo edit summary |
||
| (17 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
{{subpages}} | {{subpages}} | ||
{{TOC|right}} | |||
In [[health care]], an '''abdominal aortic aneurysm''' is "an abnormal balloon- or sac-like dilatation in the wall of the [[abdominal aorta]] which gives rise to the visceral, the parietal, and the terminal (iliac) branches below the aortic hiatus at the diaphragm."<ref>{{MeSH}}</ref> | |||
==Risk factors== | |||
*smoking | |||
*[[syphilis]] | |||
*[[tuberculosis]] | |||
== | ==Diagnosis== | ||
Various methods of diagnostic imaging can be used to measure the diameter of the aorta.<ref name="pmid22336051">{{cite journal| author=Long A, Rouet L, Lindholt JS, Allaire E| title=Measuring the maximum diameter of native abdominal aortic aneurysms: review and critical analysis. | journal=Eur J Vasc Endovasc Surg | year= 2012 | volume= 43 | issue= 5 | pages= 515-24 | pmid=22336051 | doi=10.1016/j.ejvs.2012.01.018 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22336051 }} </ref> | |||
==Screening== | ==Screening== | ||
A [[clinical practice guideline]] by the [http://www.ahrq.gov/clinic/uspstfix.htm U.S. Preventive Services Task Force (USPSTF)] 'recommends one-time screening for abdominal aortic aneurysm (AAA) by ultrasonography in men age 65 to 75 years who have ever smoked'.<ref name="pmid15684208">{{cite journal |author=U.S. Preventive Services Task Force |title=Screening for abdominal aortic aneurysm: recommendation statement |journal=Ann. Intern. Med. |volume=142 |issue=3 |pages=198-202 |year=2005 |pmid=15684208 |doi=|url=http://www.annals.org/cgi/content/full/142/3/198}}</ref><ref name="pmid15684209">{{cite journal |author=Fleming C, Whitlock EP, Beil TL, Lederle FA |title=Screening for abdominal aortic aneurysm: a best-evidence systematic review for the U.S. Preventive Services Task Force |journal=Ann. Intern. Med. |volume=142 |issue=3 |pages=203-11 |year=2005 |pmid=15684209 |doi=|url=http://www.annals.org/cgi/content/full/142/3/203}}[http://www.acpjc.org/Content/143/1/issue/ACPJC-2005-143-1-011.htm ACP Journal Club]</ref> This is a [http://www.ahrq.gov/clinic/3rduspstf/ratings.htm grade B recommendation]. An re-analysis of the meta-analysis estimated a [[number needed to treat | number needed to screen]] of approximately 850 patients.<ref name="pmid15989299">{{cite journal |author=Cinà CS, Devereaux PJ |title=Review: population-based screening for abdominal aortic aneurysm reduces cause-specific mortality in older men |journal=ACP J. Club |volume=143 |issue=1 |pages=11 |year=2005 |pmid=15989299 |doi= |url=http://www.acpjc.org/Content/143/1/issue/ACPJC-2005-143-1-011.htm}}</ref> | A [[clinical practice guideline]] by the [http://www.ahrq.gov/clinic/uspstfix.htm U.S. Preventive Services Task Force (USPSTF)] 'recommends one-time screening for abdominal aortic aneurysm (AAA) by ultrasonography in men age 65 to 75 years who have ever smoked'.<ref name="pmid15684208">{{cite journal |author=U.S. Preventive Services Task Force |title=Screening for abdominal aortic aneurysm: recommendation statement |journal=Ann. Intern. Med. |volume=142 |issue=3 |pages=198-202 |year=2005 |pmid=15684208 |doi=|url=http://www.annals.org/cgi/content/full/142/3/198}}</ref><ref name="pmid15684209">{{cite journal |author=Fleming C, Whitlock EP, Beil TL, Lederle FA |title=Screening for abdominal aortic aneurysm: a best-evidence systematic review for the U.S. Preventive Services Task Force |journal=Ann. Intern. Med. |volume=142 |issue=3 |pages=203-11 |year=2005 |pmid=15684209 |doi=|url=http://www.annals.org/cgi/content/full/142/3/203}}[http://www.acpjc.org/Content/143/1/issue/ACPJC-2005-143-1-011.htm ACP Journal Club]</ref> This is a [http://www.ahrq.gov/clinic/3rduspstf/ratings.htm grade B recommendation]. An re-analysis of the meta-analysis estimated a [[number needed to treat | number needed to screen]] of approximately 850 patients.<ref name="pmid15989299">{{cite journal |author=Cinà CS, Devereaux PJ |title=Review: population-based screening for abdominal aortic aneurysm reduces cause-specific mortality in older men |journal=ACP J. Club |volume=143 |issue=1 |pages=11 |year=2005 |pmid=15989299 |doi= |url=http://www.acpjc.org/Content/143/1/issue/ACPJC-2005-143-1-011.htm}}</ref> | ||
The largest of the [[randomized controlled trial]]s on which this guideline was based studied a screening program that consisted of<ref name="pmid12443589">{{cite journal |author=Ashton HA, Buxton MJ, Day NE, ''et al'' |title=The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial |journal=Lancet |volume=360 |issue=9345 |pages=1531-9 |year=2002 |pmid=12443589 |doi=}} [http://www.acpjc.org/Content/138/3/issue/ACPJC-2003-138-3-066.htm ACP Journal Club]</ref>: | |||
:Screening men ages 65-74 years (not restricted to ever smokers). 'Men in whom abdominal aortic aneurysms (> or =3 cm in diameter) were detected were followed-up... Patients with an aortic diameter of 3·0–4·4 cm were rescanned at yearly intervals, whereas those with an aortic diameter of 4·5–5·4 cm were rescanned at 3-monthly intervals ... Surgery was considered on specific criteria (diameter > or =5.5 cm, expansion > or =1 cm per year, symptoms)'. | |||
This trial reported significant short<ref name="pmid12443589"/> ([[number needed to treat | number needed to screen]] after 4 years of approximately 590 to prevent nonfatal ruptured AAA plus AAA-related deaths<ref name="pmid12725621">{{cite journal |author=Cina CS |title=Screening for abdominal aortic aneurysm reduced death from AAA in older men |journal=ACP J. Club |volume=138 |issue=3 |pages=66 |year=2003 |pmid=12725621 |doi=}}</ref>) and long term<ref name="pmid17502630">{{cite journal |author=Kim LG, P Scott RA, Ashton HA, Thompson SG |title=A sustained mortality benefit from screening for abdominal aortic aneurysm |journal=Ann. Intern. Med. |volume=146 |issue=10 |pages=699-706 |year=2007 |pmid=17502630 |doi=}}</ref> ([[number needed to treat | number needed to screen]] after 7 years of approximately 280 to prevent nonfatal ruptured AAA plus AAA-related deaths) benefit and cost effectiveness.<ref name="pmid12433761">{{cite journal |author=Multicentre Aneurysm Screening Study Group |title=Multicentre aneurysm screening study (MASS): cost effectiveness analysis of screening for abdominal aortic aneurysms based on four year results from [[randomized controlled trial]] |journal=BMJ |volume=325 |issue=7373 |pages=1135 |year=2002 |pmid=12433761 |doi=}} [http://www.acpjc.org/Content/139/1/issue/ACPJC-2003-139-1-024.htm ACP Journal Club]</ref> Subsequent [[randomized controlled trial]]s also found benefit: | |||
* [[number needed to treat | number needed to screen]] after 4 years of 300<ref name="pmid15757960">{{cite journal |author=Lindholt JS, Juul S, Fasting H, Henneberg EW |title=Screening for abdominal aortic aneurysms: single centre randomised controlled trial |journal=BMJ |volume=330 |issue=7494 |pages=750 |year=2005 |pmid=15757960 |doi=10.1136/bmj.38369.620162.82}} [http://www.acpjc.org/Content/143/2/issue/ACPJC-2005-143-2-039.htm ACP Journal Club]</ref> | |||
* [[number needed to treat | number needed to screen]] after and after 7 years of 563 ([http://medinformatics.uthscsa.edu/calculator/calc.shtml?calc_rx_2x2.shtml?a=47.0&b=2898&c=54.0&d=2991&row1total=2945&row2total=3045 calculation]).<ref name="pmid17514666">{{cite journal |author=Ashton HA, Gao L, Kim LG, Druce PS, Thompson SG, Scott RA |title=Fifteen-year follow-up of a randomized clinical trial of ultrasonographic screening for abdominal aortic aneurysms |journal=The British journal of surgery |volume=94 |issue=6 |pages=696-701 |year=2007 |pmid=17514666 |doi=10.1002/bjs.5780}}</ref> | |||
More recently, a clinical prediction rule may help identify patients for screening.<ref name="pmid20881774">{{cite journal| author=Greco G, Egorova NN, Gelijns AC, Moskowitz AJ, Manganaro AJ, Zwolak RM et al.| title=Development of a novel scoring tool for the identification of large ≥5 cm abdominal aortic aneurysms. | journal=Ann Surg | year= 2010 | volume= 252 | issue= 4 | pages= 675-82 | pmid=20881774 | doi=10.1097/SLA.0b013e3181f621c8 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20881774 }} </ref> | |||
===MEDICARE criteria for screening=== | |||
Effective January 1, 2007, provisions of the SAAAVE Act (Screening Abdominal Aortic Aneurysm Very Efficiently) now provide a free, one-time, ultrasound AAA screening benefit for those qualified seniors. Men who have smoked at least 100 cigarettes during their life, and men and women with a family history of AAA qualify for the one-time ultrasound screening. | Effective January 1, 2007, provisions of the SAAAVE Act (Screening Abdominal Aortic Aneurysm Very Efficiently) now provide a free, one-time, ultrasound AAA screening benefit for those qualified seniors. Men who have smoked at least 100 cigarettes during their life, and men and women with a family history of AAA qualify for the one-time ultrasound screening. | ||
| Line 17: | Line 30: | ||
The Welcome to Medicare Physical Exam must be completed within the first six months of Medicare eligibility, but there is no published time limit thereafter for completion of the AAA screening. Providers who perform the physical and order the AAA screening need to document the AAA risk factors.<ref>Society for Vascular Surgery</ref> | The Welcome to Medicare Physical Exam must be completed within the first six months of Medicare eligibility, but there is no published time limit thereafter for completion of the AAA screening. Providers who perform the physical and order the AAA screening need to document the AAA risk factors.<ref>Society for Vascular Surgery</ref> | ||
==Differential diagnosis== | |||
==Potential comorbidities== | |||
==Treatment== | |||
Indications for surgery in patients without symptoms are:<ref name="pmid18234753">{{cite journal |author=Greenhalgh RM, Powell JT |title=Endovascular repair of abdominal aortic aneurysm |journal=N. Engl. J. Med. |volume=358 |issue=5 |pages=494–501 |year=2008 |month=January |pmid=18234753 |doi=10.1056/NEJMct0707524 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=18234753&promo=ONFLNS19 |issn=}}</ref> | |||
* size greater than 5.5 cm in diameter | |||
* "becomes tender" | |||
* grows more than 1 cm in diameter per year | |||
===Surgical repair=== | |||
Repair should be considered for symptomatic aneurysms or those larger than 5.5 cm according to a systematic review<ref name="pmid17502634">Lederle FA, Kane RL, MacDonald R, Wilt TJ. Systematic review: repair of unruptured abdominal aortic aneurysm. Ann Intern Med. 2007 May 15;146(10):735-41. PMID 17502634</ref> of [[randomized controlled trial]]s.<ref name="pmid12000813">{{cite journal |author=Lederle FA, Wilson SE, Johnson GR, ''et al.'' |title=Immediate repair compared with surveillance of small abdominal aortic aneurysms |journal=N. Engl. J. Med. |volume=346 |issue=19 |pages=1437–44 |year=2002 |month=May |pmid=12000813 |doi=10.1056/NEJMoa012573 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=12000813&promo=ONFLNS19 |issn=}}</ref>><ref name="pmid12000814">{{cite journal |author=United Kingdom Small Aneurysm Trial Participants |title=Long-term outcomes of immediate repair compared with surveillance of small abdominal aortic aneurysms |journal=N. Engl. J. Med. |volume=346 |issue=19 |pages=1445–52 |year=2002 |month=May |pmid=12000814 |doi=10.1056/NEJMoa013527 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=12000814&promo=ONFLNS19 |issn=}}</ref> | |||
===Endovascular repair=== | |||
{| class="wikitable" | |||
|+ Randomized controlled trials of endovascular repair.<ref name="pmid20382983">{{cite journal| author=United Kingdom EVAR Trial Investigators. Greenhalgh RM, Brown LC, Powell JT, Thompson SG, Epstein D et al.| title=Endovascular versus open repair of abdominal aortic aneurysm. | journal=N Engl J Med | year= 2010 | volume= 362 | issue= 20 | pages= 1863-71 | pmid=20382983 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=20382983 | doi=10.1056/NEJMoa0909305 }} </ref><ref name="pmid20382982">{{cite journal| author=United Kingdom EVAR Trial Investigators. Greenhalgh RM, Brown LC, Powell JT, Thompson SG, Epstein D| title=Endovascular repair of aortic aneurysm in patients physically ineligible for open repair. | journal=N Engl J Med | year= 2010 | volume= 362 | issue= 20 | pages= 1872-80 | pmid=20382982 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=20382982 | doi=10.1056/NEJMoa0911056 }} </ref><ref name="pmid20484396">{{cite journal| author=De Bruin JL, Baas AF, Buth J, Prinssen M, Verhoeven EL, Cuypers PW et al.| title=Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. | journal=N Engl J Med | year= 2010 | volume= 362 | issue= 20 | pages= 1881-9 | pmid=20484396 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=20484396 | doi=10.1056/NEJMoa0909499 }} </ref> | |||
! !! Patients!! Intervention!! Comparison!! Outcome!! Results | |||
|- | |||
| DREAM<ref name="pmid20484396"/><br/>(2010)|| Aneurysms > 5.0 cm<br/>Mean age 70|| Endovascular|| Open repair|| Mortality at 6 yrs|| Endo=31%<br/>Open=30% | |||
|- | |||
| EVAR-1<ref name="pmid20382983"/><br/>(2010)|| Aneurysms > 5.5 cm<br/>Mean age 74|| Endovascular|| Open repair || Mortality at 6 yrs|| Endo=42%<br/>Open=42% | |||
|- | |||
| EVAR-2<ref name="pmid20382982"/><br/>(2010)|| Aneurysms > 5.5 cm<br/>Mean age 77<br/>Unfit for open repair|| Endovascular|| None|| Mortality at 3 yrs|| Endo=74%<br/>None=77% | |||
|} | |||
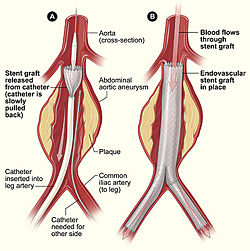
{{Image|Aneurysm endovascular.jpg|right|250px|Endovascular repair of abdominal aortic aneurysm.}} | |||
Endovascular repair (i.e., inserting a [[stent]] or patch) is a less invasive procedure that may be used when the renal arteries are not part of the aneurysm.<ref name="pmid22511690">{{cite journal| author=Jackson RS, Chang DC, Freischlag JA| title=Comparison of long-term survival after open vs endovascular repair of intact abdominal aortic aneurysm among Medicare beneficiaries. | journal=JAMA | year= 2012 | volume= 307 | issue= 15 | pages= 1621-8 | pmid=22511690 | doi=10.1001/jama.2012.453 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22511690 }} </ref> Endovascular repair has improved short term outcomes.<ref name="pmid15483279">{{cite journal |author=Prinssen M, Verhoeven EL, Buth J, ''et al.'' |title=A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms |journal=N. Engl. J. Med. |volume=351 |issue=16 |pages=1607–18 |year=2004 |month=October |pmid=15483279 |doi=10.1056/NEJMoa042002 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=15483279&promo=ONFLNS19 |issn=}}</ref> However, it has similar outcomes as compared to open surgery at two years<ref name="pmid15944424">{{cite journal |author=Blankensteijn JD, de Jong SE, Prinssen M, ''et al.'' |title=Two-year outcomes after conventional or endovascular repair of abdominal aortic aneurysms |journal=N. Engl. J. Med. |volume=352 |issue=23 |pages=2398–405 |year=2005 |month=June |pmid=15944424 |doi=10.1056/NEJMoa051255 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=15944424&promo=ONFLNS19 |issn=}}</ref> and six years<ref name="pmid20484396">{{cite journal| author=De Bruin JL, Baas AF, Buth J, Prinssen M, Verhoeven EL, Cuypers PW et al.| title=Long-term outcome of open or endovascular repair of abdominal aortic aneurysm. | journal=N Engl J Med | year= 2010 | volume= 362 | issue= 20 | pages= 1881-9 | pmid=20484396 | |||
| url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=clinical.uthscsa.edu/cite&retmode=ref&cmd=prlinks&id=20484396 | doi=10.1056/NEJMoa0909499 }} </ref>. | |||
In a [[cohort study]], endovascular repair may have improved outcomes as compared to open repair.<ref name="pmid22511690">{{cite journal| author=Jackson RS, Chang DC, Freischlag JA| title=Comparison of long-term survival after open vs endovascular repair of intact abdominal aortic aneurysm among Medicare beneficiaries. | journal=JAMA | year= 2012 | volume= 307 | issue= 15 | pages= 1621-8 | pmid=22511690 | doi=10.1001/jama.2012.453 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22511690 }} </ref> | |||
===Complications=== | |||
====Acute kidney injury==== | |||
[[Acute kidney injury]] is uncommon (less than 2% of patients) if the aneurysm is infrarenal and reimplantation of the renal arteries is not needed.<ref name="pmid15483279">{{cite journal |author=Prinssen M, Verhoeven EL, Buth J, ''et al.'' |title=A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms |journal=N. Engl. J. Med. |volume=351 |issue=16 |pages=1607–18 |year=2004 |month=October |pmid=15483279 |doi=10.1056/NEJMoa042002 |url=http://content.nejm.org/cgi/pmidlookup?view=short&pmid=15483279&promo=ONFLNS19 |issn=}}</ref> | |||
==Prognosis== | |||
==Attribution== | |||
{{WPAttribution}} | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}}[[Category:Suggestion Bot Tag]] | ||
Latest revision as of 13:54, 5 July 2024
In health care, an abdominal aortic aneurysm is "an abnormal balloon- or sac-like dilatation in the wall of the abdominal aorta which gives rise to the visceral, the parietal, and the terminal (iliac) branches below the aortic hiatus at the diaphragm."[1]
Risk factors
- smoking
- syphilis
- tuberculosis
Diagnosis
Various methods of diagnostic imaging can be used to measure the diameter of the aorta.[2]
Screening
A clinical practice guideline by the U.S. Preventive Services Task Force (USPSTF) 'recommends one-time screening for abdominal aortic aneurysm (AAA) by ultrasonography in men age 65 to 75 years who have ever smoked'.[3][4] This is a grade B recommendation. An re-analysis of the meta-analysis estimated a number needed to screen of approximately 850 patients.[5]
The largest of the randomized controlled trials on which this guideline was based studied a screening program that consisted of[6]:
- Screening men ages 65-74 years (not restricted to ever smokers). 'Men in whom abdominal aortic aneurysms (> or =3 cm in diameter) were detected were followed-up... Patients with an aortic diameter of 3·0–4·4 cm were rescanned at yearly intervals, whereas those with an aortic diameter of 4·5–5·4 cm were rescanned at 3-monthly intervals ... Surgery was considered on specific criteria (diameter > or =5.5 cm, expansion > or =1 cm per year, symptoms)'.
This trial reported significant short[6] ( number needed to screen after 4 years of approximately 590 to prevent nonfatal ruptured AAA plus AAA-related deaths[7]) and long term[8] ( number needed to screen after 7 years of approximately 280 to prevent nonfatal ruptured AAA plus AAA-related deaths) benefit and cost effectiveness.[9] Subsequent randomized controlled trials also found benefit:
- number needed to screen after 4 years of 300[10]
- number needed to screen after and after 7 years of 563 (calculation).[11]
More recently, a clinical prediction rule may help identify patients for screening.[12]
MEDICARE criteria for screening
Effective January 1, 2007, provisions of the SAAAVE Act (Screening Abdominal Aortic Aneurysm Very Efficiently) now provide a free, one-time, ultrasound AAA screening benefit for those qualified seniors. Men who have smoked at least 100 cigarettes during their life, and men and women with a family history of AAA qualify for the one-time ultrasound screening.
Enrollees must visit their healthcare professional for their Welcome to Medicare physical within six months of enrollment in order to qualify for the free screening.
The Welcome to Medicare Physical Exam must be completed within the first six months of Medicare eligibility, but there is no published time limit thereafter for completion of the AAA screening. Providers who perform the physical and order the AAA screening need to document the AAA risk factors.[13]
Differential diagnosis
Potential comorbidities
Treatment
Indications for surgery in patients without symptoms are:[14]
- size greater than 5.5 cm in diameter
- "becomes tender"
- grows more than 1 cm in diameter per year
Surgical repair
Repair should be considered for symptomatic aneurysms or those larger than 5.5 cm according to a systematic review[15] of randomized controlled trials.[16]>[17]
Endovascular repair
| Patients | Intervention | Comparison | Outcome | Results | |
|---|---|---|---|---|---|
| DREAM[20] (2010) |
Aneurysms > 5.0 cm Mean age 70 |
Endovascular | Open repair | Mortality at 6 yrs | Endo=31% Open=30% |
| EVAR-1[18] (2010) |
Aneurysms > 5.5 cm Mean age 74 |
Endovascular | Open repair | Mortality at 6 yrs | Endo=42% Open=42% |
| EVAR-2[19] (2010) |
Aneurysms > 5.5 cm Mean age 77 Unfit for open repair |
Endovascular | None | Mortality at 3 yrs | Endo=74% None=77% |
Endovascular repair (i.e., inserting a stent or patch) is a less invasive procedure that may be used when the renal arteries are not part of the aneurysm.[21] Endovascular repair has improved short term outcomes.[22] However, it has similar outcomes as compared to open surgery at two years[23] and six years[20].
In a cohort study, endovascular repair may have improved outcomes as compared to open repair.[21]
Complications
Acute kidney injury
Acute kidney injury is uncommon (less than 2% of patients) if the aneurysm is infrarenal and reimplantation of the renal arteries is not needed.[22]
Prognosis
Attribution
- Some content on this page may previously have appeared on Wikipedia.
References
- ↑ Anonymous (2024), Abdominal aortic aneurysm (English). Medical Subject Headings. U.S. National Library of Medicine.
- ↑ Long A, Rouet L, Lindholt JS, Allaire E (2012). "Measuring the maximum diameter of native abdominal aortic aneurysms: review and critical analysis.". Eur J Vasc Endovasc Surg 43 (5): 515-24. DOI:10.1016/j.ejvs.2012.01.018. PMID 22336051. Research Blogging.
- ↑ U.S. Preventive Services Task Force (2005). "Screening for abdominal aortic aneurysm: recommendation statement". Ann. Intern. Med. 142 (3): 198-202. PMID 15684208. [e]
- ↑ Fleming C, Whitlock EP, Beil TL, Lederle FA (2005). "Screening for abdominal aortic aneurysm: a best-evidence systematic review for the U.S. Preventive Services Task Force". Ann. Intern. Med. 142 (3): 203-11. PMID 15684209. [e] ACP Journal Club
- ↑ Cinà CS, Devereaux PJ (2005). "Review: population-based screening for abdominal aortic aneurysm reduces cause-specific mortality in older men". ACP J. Club 143 (1): 11. PMID 15989299. [e]
- ↑ 6.0 6.1 Ashton HA, Buxton MJ, Day NE, et al (2002). "The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial". Lancet 360 (9345): 1531-9. PMID 12443589. [e] ACP Journal Club
- ↑ Cina CS (2003). "Screening for abdominal aortic aneurysm reduced death from AAA in older men". ACP J. Club 138 (3): 66. PMID 12725621. [e]
- ↑ Kim LG, P Scott RA, Ashton HA, Thompson SG (2007). "A sustained mortality benefit from screening for abdominal aortic aneurysm". Ann. Intern. Med. 146 (10): 699-706. PMID 17502630. [e]
- ↑ Multicentre Aneurysm Screening Study Group (2002). "Multicentre aneurysm screening study (MASS): cost effectiveness analysis of screening for abdominal aortic aneurysms based on four year results from randomized controlled trial". BMJ 325 (7373): 1135. PMID 12433761. [e] ACP Journal Club
- ↑ Lindholt JS, Juul S, Fasting H, Henneberg EW (2005). "Screening for abdominal aortic aneurysms: single centre randomised controlled trial". BMJ 330 (7494): 750. DOI:10.1136/bmj.38369.620162.82. PMID 15757960. Research Blogging. ACP Journal Club
- ↑ Ashton HA, Gao L, Kim LG, Druce PS, Thompson SG, Scott RA (2007). "Fifteen-year follow-up of a randomized clinical trial of ultrasonographic screening for abdominal aortic aneurysms". The British journal of surgery 94 (6): 696-701. DOI:10.1002/bjs.5780. PMID 17514666. Research Blogging.
- ↑ Greco G, Egorova NN, Gelijns AC, Moskowitz AJ, Manganaro AJ, Zwolak RM et al. (2010). "Development of a novel scoring tool for the identification of large ≥5 cm abdominal aortic aneurysms.". Ann Surg 252 (4): 675-82. DOI:10.1097/SLA.0b013e3181f621c8. PMID 20881774. Research Blogging.
- ↑ Society for Vascular Surgery
- ↑ Greenhalgh RM, Powell JT (January 2008). "Endovascular repair of abdominal aortic aneurysm". N. Engl. J. Med. 358 (5): 494–501. DOI:10.1056/NEJMct0707524. PMID 18234753. Research Blogging.
- ↑ Lederle FA, Kane RL, MacDonald R, Wilt TJ. Systematic review: repair of unruptured abdominal aortic aneurysm. Ann Intern Med. 2007 May 15;146(10):735-41. PMID 17502634
- ↑ Lederle FA, Wilson SE, Johnson GR, et al. (May 2002). "Immediate repair compared with surveillance of small abdominal aortic aneurysms". N. Engl. J. Med. 346 (19): 1437–44. DOI:10.1056/NEJMoa012573. PMID 12000813. Research Blogging.
- ↑ United Kingdom Small Aneurysm Trial Participants (May 2002). "Long-term outcomes of immediate repair compared with surveillance of small abdominal aortic aneurysms". N. Engl. J. Med. 346 (19): 1445–52. DOI:10.1056/NEJMoa013527. PMID 12000814. Research Blogging.
- ↑ 18.0 18.1 United Kingdom EVAR Trial Investigators. Greenhalgh RM, Brown LC, Powell JT, Thompson SG, Epstein D et al. (2010). "Endovascular versus open repair of abdominal aortic aneurysm.". N Engl J Med 362 (20): 1863-71. DOI:10.1056/NEJMoa0909305. PMID 20382983. Research Blogging.
- ↑ 19.0 19.1 United Kingdom EVAR Trial Investigators. Greenhalgh RM, Brown LC, Powell JT, Thompson SG, Epstein D (2010). "Endovascular repair of aortic aneurysm in patients physically ineligible for open repair.". N Engl J Med 362 (20): 1872-80. DOI:10.1056/NEJMoa0911056. PMID 20382982. Research Blogging.
- ↑ 20.0 20.1 20.2 De Bruin JL, Baas AF, Buth J, Prinssen M, Verhoeven EL, Cuypers PW et al. (2010). "Long-term outcome of open or endovascular repair of abdominal aortic aneurysm.". N Engl J Med 362 (20): 1881-9. DOI:10.1056/NEJMoa0909499. PMID 20484396. Research Blogging.
- ↑ 21.0 21.1 Jackson RS, Chang DC, Freischlag JA (2012). "Comparison of long-term survival after open vs endovascular repair of intact abdominal aortic aneurysm among Medicare beneficiaries.". JAMA 307 (15): 1621-8. DOI:10.1001/jama.2012.453. PMID 22511690. Research Blogging.
- ↑ 22.0 22.1 Prinssen M, Verhoeven EL, Buth J, et al. (October 2004). "A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms". N. Engl. J. Med. 351 (16): 1607–18. DOI:10.1056/NEJMoa042002. PMID 15483279. Research Blogging.
- ↑ Blankensteijn JD, de Jong SE, Prinssen M, et al. (June 2005). "Two-year outcomes after conventional or endovascular repair of abdominal aortic aneurysms". N. Engl. J. Med. 352 (23): 2398–405. DOI:10.1056/NEJMoa051255. PMID 15944424. Research Blogging.